The digital era provides a huge opportunity to innovate in the field of health and care. COVID-19 accelerated the need to re-engineer health systems and leverage the power of digital and Artificial Intelligence (AI) to make them become proactive, predictive and ultimately preventative.
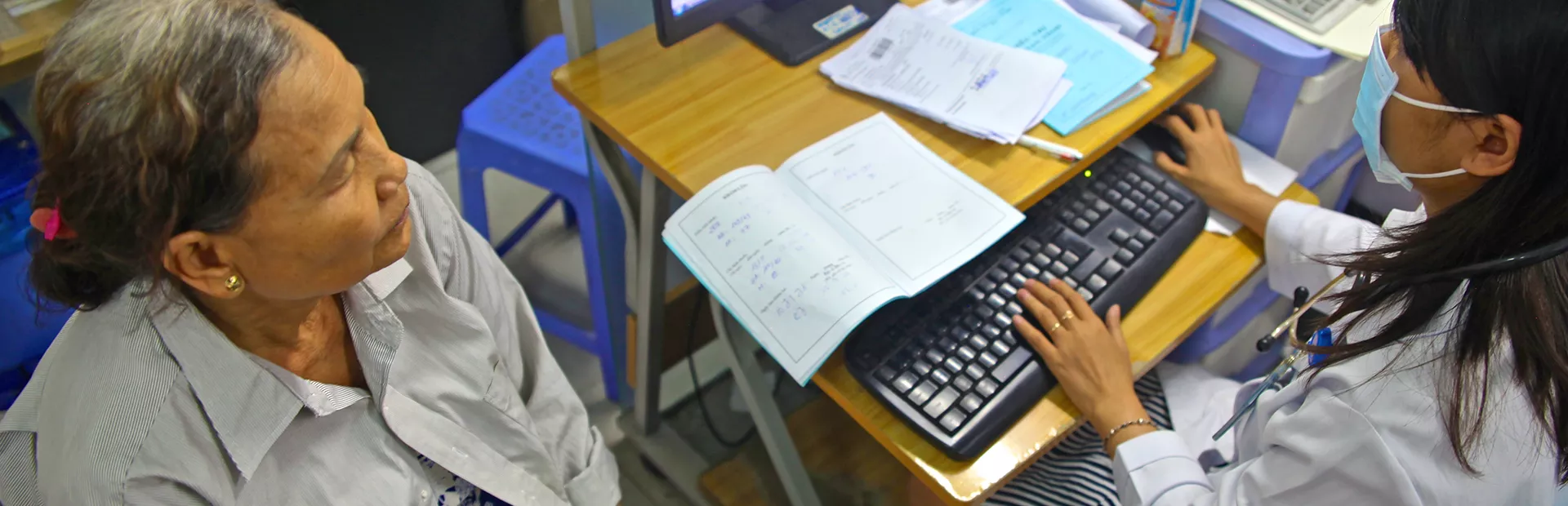
Beside the collection and use of real-time data, digital technology provides an array of opportunities to transform the way health and care are delivered. Health systems can tap into the potential of digital even when no digital health information system or electronic health record system exists. Yet, for digital health solutions to reach scale and impact, they should be needs-driven, human-centered and developed iteratively – for and with end users. Importantly, they have to be tailored to the local context, use the available infrastructure, and integrated in the health ecosystem and workflows. Examples of digital solutions that can deploy without a highly mature digital health system include:
- Virtual care (telehealth) has proven vital during the COVID-19 pandemic, with several health systems making strides in its use. Telehealth can deliver a true paradigm shift for outpatient care, benefitting primary care services (provider-to-provider, bringing specialist advice into the core of care, at the frontline) through tools for group consultations, self-care, remote appointments and follow-up. It can also enable structured triage, optimize consultation times and even increase diagnosis accuracy by ensuring referral tests happen before appointments.
- Bluetooth-enabled devices or mobile camera-based blood pressure measurement can significantly accelerate hypertension detection and timely diagnosis. Such digital services can create access, streamline the CV risk screening outside the hospital in high-traffic venues across cities and appropriately funnel within the health system individuals who screened positive.
- On one side, digital tracker apps allow health professionals to monitor screening, diagnosis and treatment progress – enabling them to take decisions based on real-time information. On the other side, such digital assistants empower individuals to manage better their health through simple SMS, chat or voice messages, complemented by notifications for follow-up appointments and medication reminders.
- Online continuous medical education and distance learning through mobile devices and computers help train and upskill health professionals and their community partners.
- Social media platforms, including WhatsApp and Facebook, deliver health literacy through interactive content and mass chats, and can build the foundation for smart chatbot assistants that help in the triage of patients.
When the data collected through digital solutions and devices is made accessible and successfully integrated, it can serve as the ‘fuel’ for data-driven health system analytics and predictive models. Also, collecting data on the main interventions a city chooses as its CV population health approach is fundamental to monitoring both progress and impact.
Transitioning from paper-based data collection to digital collection through the implementation of digital health information systems (HIS) is critical to steer health policy with real-time data. Digitized HIS provide the foundation to optimize operations and transform care systems into health systems that keep their populations healthy.
Findings from data analytics can lead to unbiased, evidence-based population health policy and actions that improve lives and transform health systems. AI models can highlight which interventions would generate the largest population health impact. They will not only map the determinants of health on an individual level but also help remove health inequalities by enabling policy makers to establish frameworks for data-informed decisions and innovation through novel HealthTech solutions and services.
The successful digitization of HIS is based on multiple prerequisites: a reliable broadband connection and infrastructure, strengthening data and digital skills of health workers and their managers, establishing a clear data strategy including interoperability standards, data privacy and security by design, governance models, regulations and processes. Whether it is a primary health center (PHC), a regional hospital or a specialized referral center, connectivity and interoperability, a digitally-savvy workforce and well-established standards and procedures are key to providing coordinated care across all levels of the health system. Ideally, digital health information systems should allow people to have full visibility and control of their own health data, so they can mindfully share it with health providers and researchers.